Alzheimer’s Disease: Signs, Symptoms, and Causes
Recognizing the symptoms and coping with a diagnosis

The earlier you can detect Alzheimer's Disease, the better your treatment options. Here’s how to spot the early warning signs in yourself or a loved one and get an accurate diagnosis.

Adapted with permission from Alzheimer's Disease: A guide to diagnosis, treatment, and caregiving, a special health report published by Harvard Health Publishing.
Alzheimer's Disease can be caught in the early stages—when the best treatments are available—by watching for telltale warning signs. If you recognize the warning signs in yourself or a loved one, make an appointment to see your physician right away. Brain imaging technology can diagnose Alzheimer's early, improving the opportunities for symptom management.
Alzheimer’s disease usually is not diagnosed in the early stages, even in people who visit their primary care doctors with memory complaints.
Recognizing symptoms early is crucial because medication to control symptoms is most effective in the early stages of the disease and early diagnosis allows the individual and his or her family members to plan for the future. If you or a loved one is experiencing any of the following symptoms, contact a physician.
Progressive memory loss. This is the hallmark of Alzheimer’s disease. Initially, only short-term memory is impaired, and the person merely seems forgetful. But because short-term memory is essential for absorbing new information, the impairment soon interferes with the ability to interact socially and perform one’s work. Long-term memory may be retained longer, often in great detail, but it becomes fragmented as the disease progresses. Toward the final stage, people with Alzheimer’s may be unable to recall their own names.
Decline in cognitive abilities. These are the “thinking” activities of reasoning—solving problems, making decisions, exercising judgment, and so on. Impairments of cognitive function can begin subtly as poor performance in an activity the person once did well. Poor judgment and lack of insight can lead to accidents.
Early in the disease, individuals may easily lose track of time; later, their disorientation becomes more pronounced and extends to places and people. The sense of time becomes more distorted as the disease progresses, and people may insist it’s time to leave immediately after arriving at a place or may complain of not having been fed as soon as a meal has ended.
Changes in mood and personality. These changes are often the most convincing evidence for families that something is wrong. Apathy is common, and many individuals lose interest in their usual activities. A person may become withdrawn, irritable, or inexplicably hostile.
Depression may also accompany Alzheimer’s, partly as a result of chemical changes in the brain caused by the disease itself and partly as an understandable psychological reaction to the loss of mental abilities. Symptoms of depression include loss of interest in previously enjoyable activities, change in appetite that sometimes leads to weight loss or gain, insomnia or oversleeping, loss of energy, and feelings of worthlessness. People with Alzheimer’s, though, seldom have feelings of excessive guilt or thoughts of suicide, which are often symptoms of depression.
Aphasia. This medical term describes an impairment in using and understanding language. Because speaking, writing, reading, and understanding speech involve different areas of the brain and different nerve networks, aphasia can be uneven, with some skills retained longer than others. For example, a person may be able to recognize written words flawlessly and yet fail to comprehend their meanings.
Typically, aphasia begins with word-finding difficulties. Unable to think of the right words, a person may try to cover up with long-winded descriptions that fail to reach the point, or he or she may angrily refuse to discuss the matter further. Substituting a similar-sounding word (“wrong” instead of “ring”) or a related word (“read” instead of “book”) is common. The person may ramble, stringing phrases together without expressing any real thought, or may forget all but a few words (which he or she may repeat over and over). In many cases, all language abilities are lost as dementia becomes severe, and people become mute.
Agnosia. The ability to process sensory information deteriorates, causing agnosia, a disorder in perception. Unable to comprehend the meaning of what they see, people with agnosia may run into furniture. They may believe a spouse is an impostor, become frightened by ordinary sounds, or fail to recognize their own reflection in a mirror. Agnosia can contribute to inappropriate behavior, such as urinating into a wastebasket.
Apraxia. The inability to perform basic motor skills such as walking, dressing, and eating a meal is known as apraxia. This is quite different from weakness or paralysis caused by a stroke. A person with apraxia has literally forgotten how to perform these activities. Usually, apraxia develops gradually, but in some cases, it begins abruptly. Apraxia may first be evident in fine hand movements, showing up in illegible handwriting and clumsiness in buttoning clothing. Everyday skills like using a phone or switching channels on a TV set may disappear. Eventually the ability to chew, walk, or sit up in a chair is lost.
Behavior problems. Troublesome changes in behavior are a common feature of the disease. Examples include being stubborn, resisting care, refusing to give up unsafe activities, pacing or hand-wringing, wandering, using obscene or abusive language, stealing, hiding things, getting lost, engaging in inappropriate sexual behavior, urinating in unsuitable places, wearing too few or too many clothes, eating inappropriate objects, dropping lit cigarettes, and so on. A particular behavior can disappear as a patient’s abilities further deteriorate (for example, verbal abuse declines as aphasia progresses), only to be replaced with new problems.
Catastrophic reaction. A strong emotional response to a minor problem is another symptom of the disease. Catastrophic reactions can involve crying inconsolably, shouting, swearing, agitated pacing, refusing to participate in an activity, or striking out at another person. The usual triggers include fatigue, stress, discomfort, and the failure to understand a situation. Essentially, a catastrophic reaction is the response of an overwhelmed, frightened person who feels cornered and is trying to protect himself or herself. The behavior is caused by brain dysfunction and is mostly beyond the person’s control.
Sundowning. This term refers to behavior problems that worsen in the late afternoon and evening. No one knows exactly why sundowning occurs, though there are several theories. Because people are tired at the end of the day, their tolerance for stress declines, and a minor problem can generate a major outburst. An already confused person may be overstimulated when several people are in the house, dinner preparations are under way, and the television is on. Dim light may also contribute to a person’s misinterpretation of visual information.
Psychosis. Roughly four out of 10 people with Alzheimer’s disease will experience psychosis, which is marked by recurring delusions or hallucinations. While this most often occurs in late-onset Alzheimer’s and appears to run in families, specific genes associated with it have not yet been pinpointed. The disordered thinking that prompts delusions and hallucinations occurs sporadically, which tends not to be true in other forms of psychosis.
A woman troubled by delusions might call the police to report strangers in the house, talk to herself in the mirror, or talk to people on TV. Hallucinations are often visual—seeing jagged rocks or water where floorboards actually are—but may be auditory (phantom voices), as well.
No blood test, brain scan, or physical exam can definitively diagnose Alzheimer’s disease. And because so many conditions can produce symptoms resembling those of early Alzheimer’s, reaching the correct diagnosis is complicated.
It’s important to find a physician experienced in Alzheimer’s diagnosis. If a physician diagnoses Alzheimer’s after only a cursory examination, get a second opinion. A complete evaluation by a specialist is essential to exclude other health problems that could cause cognitive problems. Your family physician may do part of the evaluation and then recommend a neurologist, geriatrician, or other specialist to complete it. Your local Alzheimer’s Association chapter, medical school, or hospital can also identify appropriate specialists.
Before scheduling an appointment, ask what diagnostic procedures will be used. If the evaluation does not sound comprehensive, seek another physician.
Once a diagnosis is made, find a physician experienced in providing ongoing care to meet the changing needs of someone with Alzheimer’s disease. The doctor who makes the diagnosis may not be the one who will oversee the long-term care. So, try to choose a physician who’s knowledgeable about managing dementing illnesses and able to communicate well with family members.
Families sometimes encounter a major stumbling block when the person whose mental status has aroused concern
refuses to see a doctor. Often the person denies having cognitive difficulties and resists visiting a doctor
for evaluation. In this case, arranging a doctor’s visit for a more general purpose, such as a routine
physical exam, or for a specific complaint, such as a headache, might pro- vide an opportunity to begin the
Alzheimer’s evaluation. Call the doctor in advance to inform him or her that this is one purpose for the
visit.
A complete evaluation will take more than a day and is generally done on an outpatient basis. In most areas, the evaluation can be done locally, and tests can be spread over several days to avoid tiring the person being examined. Other specialists besides the treating physician may be involved in the evaluation, including technicians, nurses, psychologists, occupational or physical therapists, social workers, and often psychiatrists.
It will take several days before test results are reported and the physician reviews them. When the doctor discusses the findings, be prepared for an equivocal diagnosis. Physicians are often hesitant to diagnose Alzheimer’s disease without first observing that the dementia is progressive. This means repeating the evaluation, usually in six to 12 months. At this later time, a more confident diagnosis is sometimes possible, but when cognitive changes are gradual, the doctor may recommend repeated testing at yearly intervals.
To help alleviate any stress associated with your visit to the physician, it’s best to be as prepared as possible. For instance, be sure that whoever goes with the individual being evaluated is familiar with his or her medical history, current symptoms, and concerns.
Beforehand, write down any issues you want to mention at the visit. If the person is in an advanced stage of dementia, you may want to bring a music player with headphones to play calming music, or a familiar soft item that can be stroked or held.
The physician will need the following:
This may seem like a lot of information, but the person’s history enables the physician to construct a list of possible diagnoses that will guide the medical evaluation that follows. For example, a physician who usually schedules a computed tomography (CT) or magnetic resonance imaging (MRI) scan of the brain as a final test might order one immediately for someone with abrupt mental changes and difficulty walking. These symptoms might indicate excess cerebrospinal fluid around the brain, a condition called normal-pressure hydrocephalus (see “Brain scans,” below). Prompt detection and treatment could prevent permanent damage to the brain.
Disorders as diverse as heart failure, liver disease, kidney failure, thyroid disorders, and respiratory diseases can cause dementia-like changes. What’s more, elderly people don’t always have typical symptoms. The sensation of pain is often dulled in the older person, for example, and it’s not unusual for confusion, rather than chest pain, to be the main symptom of a heart attack.
Therefore, the physician will evaluate the cardiovascular system, lungs, and other organs for any signs of abnormalities. Because sensory losses can add significantly to a person’s cognitive difficulties, the doc- tor will also test vision and hearing. The physician will also pay close attention to the nervous system, because neurologic abnormalities may signal a brain disorder other than Alzheimer’s disease.
Muscle strength, coordination, reflexes, senses, eye movement, and the pupils’ reaction to light can tell the physician about the health of specific areas of the brain. For example, unequal reflexes or weakness on one side of the body suggest localized brain damage (perhaps from stroke or tumor), while tremors or other involuntary movements may indicate a degenerative disorder such as Parkinson’s disease. These types of abnormalities are not usually features of early Alzheimer’s disease.
Mental status testing, which is part of the neurologic examination, is crucial in diagnosing dementia and delirium. The physician will ask the person to perform simple mental exercises such as counting backward by sevens, obeying written instructions, memorizing words, and copying designs. This testing of mental status allows the physician to assess orientation, memory, comprehension, language skills, and ability to perform simple calculations.
The physician will order a complete blood count and blood chemistry tests to detect anemia, infection, diabetes, and kidney and liver disorders. Other lab work will include routine tests for thyroid function, vitamin B12 deficiency, and elevated blood calcium, as well as a test for syphilis. If the physician suspects a specific medical problem, she may order additional tests. For example, a patient who might have been exposed to the AIDS virus will be encouraged to have an HIV test.
A brain scan—using either computed tomography (CT) or magnetic resonance imaging (MRI)—is generally included in the standard evaluation for Alzheimer’s disease and other forms of dementia.
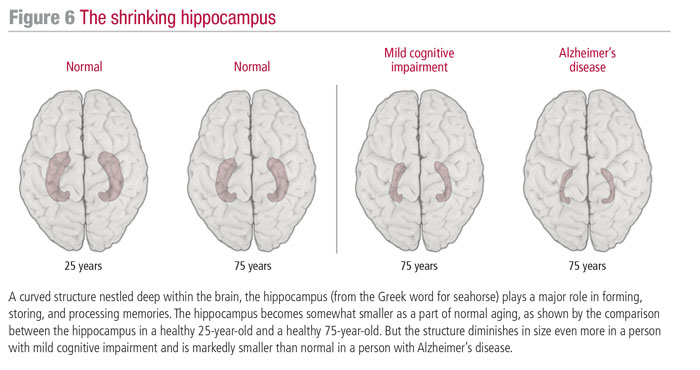
CT and MRI scans, which reveal the anatomic structure of the brain, are used to rule out such problems as tumor, hemorrhage, stroke, and hydrocephalus, which can masquerade as Alzheimer’s disease. These scans can also show the loss of brain mass associated with Alzheimer’s disease and other dementias. In Alzheimer’s disease, the region of the brain known as the hippocampus may be disproportionately atrophied.
Other brain scans may be performed if CT and MRI scans are inconclusive. Positron emission tomography (PET) and single-photon emission computed tomography provide images of brain activity based on blood flow, oxygen consumption, or glucose use. These techniques can help narrow down a diagnosis by revealing deficits common in Alzheimer’s disease that are distinct from findings for other dementias, such as frontotemporal lobar degeneration and dementia with Lewy bodies. However, even these scans cannot reveal the microscopic changes in brain tissue that characterize Alzheimer’s disease. Thus, they can’t identify the disease with certainty.
Fortunately, the diagnostic capability of brain scans is improving. Especially promising is a kind of PET scan that uses a chemical tracer that binds specifically to amyloid deposits in the brain, allowing them to show up clearly on the brain scans. Today, at least 17 centers in North America, as well as 21 others throughout the world, have successfully used one such tracer, Pittsburgh Compound-B (PiB PET), in thousands of subjects. So far, this technique is being used only in research studies. Experts anticipate PET scans with similar tracer compounds will be in general use within the next several years. These tests may help doctors diagnose the disease before symptoms appear, as well as assess new treatments.
Researchers also hope to perfect MRI techniques that can enhance physicians’ ability to measure brain atrophy and diagnose Alzheimer’s with greater accuracy. Functional MRI (fMRI), which records blood flow changes linked to brain activity, may prove helpful in distinguishing among different forms of dementia.

An electroencephalogram (EEG) may be done to detect abnormal brain-wave activity. Although the EEG is usually normal in people with mild Alzheimer’s disease and many other types of dementia, EEG abnormalities do occur in delirium and Creutzfeldt-Jakob disease, which is a cause of dementia.
If hydrocephalus (excess cerebrospinal fluid in the area around the brain) or infection of the central nervous system is suspected, the doctor may recommend a lumbar puncture to detect increased pressure or inflammatory cells in the spinal fluid. Biochemical markers for Alzheimer’s—including amyloid plaques, neurofibrillary tangles, and neurodegeneration—can also be detected. These markers are sensitive detectors of Alzheimer’s pathology, and specific for them. While tests for these markers are not commonplace today, experts anticipate that they will become a standard part of diagnostic testing in the future.
Psychologists or neuropsychologists (psychologists with specialized training in brain disorders) may administer comprehensive neuropsychological tests, either as interviews or as paper-and-pencil tests. These tests, which take several hours, are used to determine what areas of cognitive function are impaired and what areas are still intact. They assess memory, reasoning, writing, vision-motor coordination, comprehension, and the ability to express ideas. A doctor may also give other tests to identify depression and other mood problems.
Cognitive problems affect a person’s daily functioning in many different and sometimes surprising ways. An objective assessment can help determine what a person can and cannot do. This information is invaluable for caregivers, especially when the individual has other health problems that complicate the situation, such as arthritis or poor vision. If the person seems to have Alzheimer’s, a functional assessment can help determine its stage, which can help family members decide what type of care and support services are needed.
In a functional assessment, the therapist asks a family member to fill out a questionnaire about the person’s ability to perform activities of daily living. By noting what activities the person completes successfully, partially, or not at all, the therapist can suggest ways of helping the individual accomplish these tasks, thereby preserving as much of the patient’s independence as possible.
The psychosocial evaluation is usually conducted by a social worker and is designed to help the individual’s family plan for care. The social worker will discuss the emotional, physical, and financial impact of Alzheimer’s disease and guide family members through an evaluation of their circumstances. Social workers can also help coordinate community services, suggest alternatives to the person’s present living arrangements, and provide a list of resources and locally available services.
The doctor may call for a blood test in cases where there’s a family history of early-onset Alzheimer’s. To date, genetic testing offers diagnostic value only in cases of early-onset familial Alzheimer’s disease. Searching for genetic mutations in individuals who do not have a strong family history of Alzheimer’s and who did not show symptoms before age 65 is fruitless. The test for the ApoE genotype can increase diagnostic confidence somewhat, but it isn’t recommended for screening purposes.
Adapted with permission from Alzheimer's Disease: A guide to diagnosis, treatment, and caregiving, a special health report published by Harvard Health Publishing.
Last updated or reviewed on February 23, 2023Millions of readers rely on HelpGuide.org for free, evidence-based resources to understand and navigate mental health challenges. Please donate today to help us save, support, and change lives.
Donate to HelpGuide.org today